Kasai
Procedure in the Management of Biliary Atresia
Mo
Tualeka, Muqodriyanto, Ahmad Afandi, Erwin Haryono
Translator: Adrian Salim, Andrio
Wishnu Prabowo, Arnetta Naomi L. Lalisang, Julistian, Muliyadi, Sony Sanjaya,
Stefanny, Zamzania Anggia Shalih.
General
Surgery, Department of Surgery, Faculty of Medicine University of Indonesia/
Ciptomangunkusumo Hospital, Jakarta, Indonesia
Case
Illustration
A male baby, aged
2months presented with the chief complaints of jaundice in the whole body since
the age of one month, bloated abdomen, and sometimes accompanied by vomiting
milk, pale feces, and tea-colored urine.
The physical
examination showed that the baby was awake and alert, although with decreased
activities. His vital signs were still within normal limits. The eye sclera
were jaundiced, the skin was jaundiced extending to the legs. The abdomen was
distended, with enlarged veins; the liver was palpable 4 cm below the costal
arch with rubbery consistency.
The laboratory
examination revealed: total bilirubin level of 14.34 mg/dL, direct bilirubin of
9.66 mg/dL, Indirect bilirubin of 4.68 mg/dL, Leukocyte count of 14,400/mm2,
G6PD of 162 mg/dL, SGOT of 96 mgl, SGPT 14 mg/dL, Hb 10 mg/dL, and 12 mg/dL after correction.
Abdominal US: The
images of biliary atresia, hepatomegaly, and ascites. Signs of portal
hypertension were not observed
Hepatic biopsy revealed
hard fibrotic cholestasis with extrahepatic biliary atresia.
The patient was
diagnosed with Biliary Atresia and was admitted for surgery preparation.
Operation
Report:
Laparotomy with
supraumbilical transversal incision was performed, and the peritoneum was
exposed. The liver was observed to be hard with the image of cholestasis.
The gallblader was very
atretic. Holangiography was performed, there were no biliary ducts. There was
no passage of contrast in the liver and duodenum.
It was decided to
perform Kasai Procedure: The liver was liberated by cutting the ligaments and
hepatic portal was dissected, bypass portojejunostomy was performed, in which
the jejunum was cut 20 cm from the Treitz ligament, the distal jejunum was then
anastomosed with the hepatic portal, then roux-enzyme Y jejuno-jejunostomy
anastomosis was made 40 cm away from the
hepatic portal. The abdominal cavity was washed until it was clean, bleeding
was controlled, and abdominal cavity was closed layer-by-later. The surgery
lasted for 5 hours and 30 minutes.
Post-operation
The patient was
admitted to the ICU for stabilization; on day 5 of hospitalization, the patient
was moved to the patient ward. He was hospitalized for 17 days, during which he
underwent hipoalbuminemia, anemia, melena and diarrhea. Corrections of these
conditions have been performed. The patient was then discharged in good
condition, without fever and vomiting, adequately breastfed, normal defecation
and urination. However the patient was still jaundiced, with the total
bilirubin level of 12.51 mg/dL, direct bilirubin level 10.07 mg/dL, indirect
bilirubin 2.44 mg/dL. His treatment was continued in Ciptomangunkusumo Hospital
Outpatient Clinic.
Discussion
Due to the
impossibility to differentiate various etiologies of neonatal cholestasis, the
evaluation should determine the anatomical causes or obstruction in jaundice,
including biliary atresia, biliary duct
cyst, or spontaneous perforation of the biliary tract. There are numerous
non-surgical causes of neonatal jaundice, including cholangitis, metabolic,
genetic, and toxic causes.
There are three types
of Biliary Atresia:
1. Type I : atresia of
the common bile duct
2. Type II : atresia of
the common hepatic duct
3. Type III : atresia
of the left and right hepatic duct.
The patient was
diagnosed with Type III Biliary Atresia based on the clinical findings and
supporting examination, primarily intraoperative cholangiography.
Jaundice in infants persisting
for >2 weeks is not considered physiologic, especially if the main fraction
found is conjugated/direct bilirubin. Infants with biliary atresia usually looks
normal at birth, and become jaundiced at the age of 306 weeks. The color of
their feces may be normal, or might be yellow initially but changed to pale
yellow or to clay colored. Urine may become dark or tea-colored.
Laboratory In biliary
atresia, hyperbilirubinemia is observed, usually with the level of 6-12 mg/dL,
50% of which was conjugated. Transaminase and phosphatase alkaline is increased
2-3 times its normal level. The ϒ-glutamil transpeptidase is usually high.
Ultrasonography usually showed the
small or invisible gallbladder. The biliary duct was invisible and the liver
may have increased echogenicity. Hepatobiliary imaging could be performed using
technetium-99m. Iminodiacetic acid (IDA) is beneficial to differentiate
obstructive from parenchymal jaundice. In biliary atresia, especially in its
early stage, the nucleotide uptake is rapid, but there is no excretion to the
intestines.
Liver biopsy showed
proliferation of the biliary tract, portal and periportal inflammation.
Fibrosis spreading between the branches of portal suggests the development of
early cirrhosis.
Cholangiography is the final diagnostic measures usually
performed as the initial step prior to the portoenterostomy. From the small side of the right upper
quadrant, the wrinkled gallbladder will be visible. Usually the gallbladder
lacks of lumen, or only has a small lumen containing several drops of clear
fluid. Contrast demonstration to the duodenum and continuity with intrahepatic biliary
duct will exclude biliary atresia. If cholangiography is not possible (the
lumen of gallbladder was nonexistent or obstructed), the incision is enlarged
to bilateral subcostal laparotomy to prepare for Kasai portoenterostomy
Kasai
Procedure
The only therapy that gives hope of a cure for biliary
atresia is surgery. the only procedure that provides long-term success is
portoenterostomi (kasai procedure) and liver transplantation.
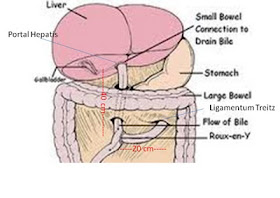
Portoenterostomi procedure begins with the mobilization of
the liver and gallblader, the dissection of the cystticus duct into the common
bile duct residual fiber (Figure 1). the Peritoneum is opened to show the
hepatic artery and biliary structures. The fibrous of communal duct is
carefully cut dissection continued proximally.
Cysticus artery was ligated. be careful to avoid misidentification of the right
hepatic artery.
Fibrous bile duct extends into cone-shaped mass and enters the liver between the bifurcation and the portal vein (figure 2). the branches of small vein must be divided carefully. the cone-shaped fibrous is cut exactly at same way with the substance of the liver (figure 3). there is no cutting cautery is used at the hilus.
Fibrous bile duct extends into cone-shaped mass and enters the liver between
the bifurcation and the portal vein (figure 2). the branches of small vein must
be divided carefully. the cone-shaped fibrous is cut exactly at same way with
the substance of the liver (figure 3). there is no cutting cautery is used at
the hilus.
Referensi :
1. * Oldham, Keith T. et all (eds); Biliary Atresia at Principles and Practice of Pediatric Surgery, 4th Edition
2. * Karrer, F. M. & Pence, J. C.; Atresia Bilier at http://www.ningrumwahyuni.files.wordpress.com/2010/03
* Glossary of Medical Terms in Biliary Atresia Research Consortium; http://www.barcnetwork.org/families/terms.html
* Biliary Atresia (Pediatric Gallbladder and BT) in http://imaging.consult.com/image/topic/dx/Gastrointestinal?title=Biliary%20Atresia%20%28Pediatric%20Gallbladder%20and%20BT%29&image=fig4&locator=gr4&pii=S1933-0332%2806%2970865-5